Osteoarthritis
Osteoarthritis is the most common cause of joint pain and dysfunction throughout the world.
What is Osteoarthritis?
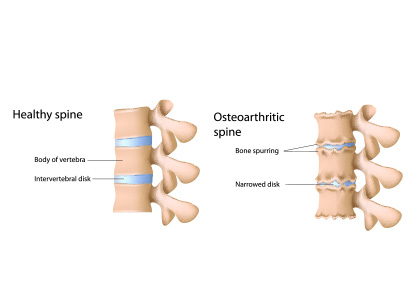
Osteoarthritis is the most common cause of joint pain and dysfunction throughout the world. The main problem leading to osteoarthritis is the loss of normal cartilage. Cartilage is the material in joints that allows bones to work smoothly together without pain. The loss of cartilage can be caused by repetitive joint trauma, or by the normal aging process (most common). It is not known why some individuals develop severe osteoarthritis without any particular risk factors.
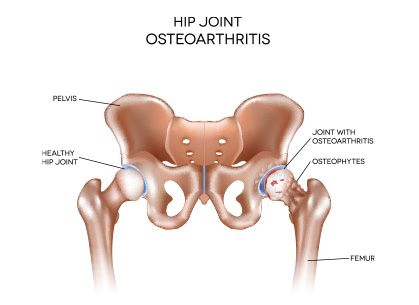
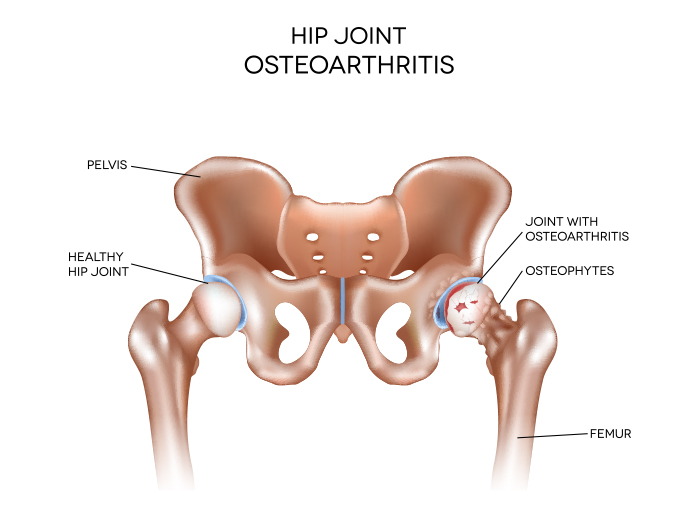
Osteoarthritis may affect any joint; and most commonly affects the hands, knees, hips and spine.
At the present time there is no cure for osteoarthritis. The symptoms can be treated, although the loss of cartilage within affected joints cannot be reversed. Treatment of osteoarthritis involves the appropriate program of treatments, that should be individualized to an individual’s specific circumstances. Treatment options include weight management, rehabilitation and physical therapy, joint interventions, pain management with analgesics, and orthopedic surgery (such as joint replacement technologies).
Eventually, the cartilage degeneration can become so severe that there is no “cushion” between the two bone surfaces that form the joint. Osteoarthritis can also affect the supporting structures of the joint, such as ligaments, tendons, and other tissues that help the joint to stay in place during movement. This progression of the illness can make the joint damage accelerate, weaken the muscles around the joint, and predispose to weakness and falls.
The symptoms of osteoarthritis are usually very mild at the beginning, and progress gradually over time. The pace of progression varies with each individual. Signs and symptoms of osteoarthritis include pain, stiffness, tenderness, loss of movement, new sensations in the joint (“grinding”, “crackling”, “clicking”, “popping”), swelling, fluid in the joint, and a larger appearance of the joint (this is known as “hypertrophy”).
Risk factors
Factors that can increase your risk of osteoarthritis include:
- The risk of getting arthritis increases with age.
- Women are more likely to develop osteoarthritis.
- The extra load associated with body habitus has an effect on the weight bearing joints, especially the hips and knees. The added load can cause extra stress on these joints and increase the risk of arthritis. It is also believed that extra fat causes inflammation that increases the risk of joint inflammation.
- There is a risk of arthritis in a joint that has been injured. Many times, the injury will heal normally and function will completely return (such as a sports injury), and arthritis will develop in the joint many years later.
- Repetitive joint stress.It is believed that certain individuals are predisposed to the development of arthritis in joints that are used repetitively in sports or during work.
- If you have a family history of severe arthritis, it is believed that your risk for arthritis is increased.
- Inherited conditions.Osteoarthritis develops more commonly in individuals born with disorders of bone, muscle, and connective tissue.
- Certain metabolic diseases.Many conditions, especially diabetes and gout, are associated with a build-up of certain chemicals can lead to joint problems that are very similar to osteoarthritis.
Complications
The primary complications associated with osteoarthritis include chronic pain, stiffness and loss of normal function. Simple activities that were once part of an individuals normal routine may become exceedingly difficult. The increased risk of falls is associated with other secondary complications such as fractures, head trauma, and the complications associated with the recovery of such unfortunate events.
Other secondary complications include anxiety (due to the risk of dropping objects, or falling), depression (due to the loss of normal recreational and occupational function) and sleep disturbances as a result of pain that repeatedly awakens individuals at night.
When to see ROC for osteoarthritis:
If you have joint pain or stiffness that is worse than usual, ROC can assist with flare-ups of osteoarthritis. An X-ray can determine whether there is a new fracture and measure the severity of the joint problem. Treatments may include joint injections, physical therapy, the use of supportive aids (including braces), and referral for a specialized Orthopaedic evaluation.